uveitis conjunctivitis keratitis
- Keywords:: Step 3, Medicine, eye disorders, conjunctivitis
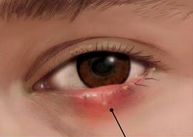
Anterior uveitis (iritis) is characterized by pain, redness, variable visual loss, and a constricted and irregular pupil.
Most cases are due to an underlying infection (eg, AIDS) or systemic inflammatory disease. Manifestations typically include:
- Erythema at the limbus (junction of cornea and sclera)
- A constricted pupil
- Blurred vision
- Moderate eye pain
To properly distinguish iritis from other causes of a red eye, it is important to visualize the anterior segment of the eye with slit lamp examination. If leukocytes are seen in the anterior segment, which contains the aqueous humor found between the cornea and the lens, then the diagnosis of iritis is confirmed. A hazy "flare," which is indicative of protein accumulation secondary to a damaged blood-aqueous barrier, may also be seen.
Patients with suspected anterior uveitis should be referred to an ophthalmologist for diagnosis. Investigation of the underlying cause is then required. Patient with bilateral hilar lymphadenopathy, erythema nodosum, anterior uveitis likely has sarcoidosis.
Treatment for iritis depends on the etiology of the condition, and typically includes antimicrobial therapy for viral or bacterial causes and topical corticosteroids for noninfectious causes. uveitis conjunctivitis keratitis
Keratitis
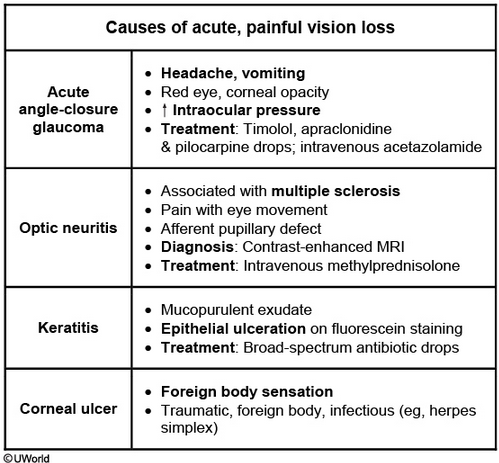
Keratitis is an inflammation of the cornea, the clear tissue covering the pupil and iris and bordered by the bulbar conjunctivae. Infectious keratitis can be due to a variety of organisms, including bacteria (eg, Pseudomonas aeruginosa), viruses (eg, herpes simplex virus, varicella-zoster virus), fungi, or parasites (eg, Acanthamoeba).
This patient with conjunctivitis has now developed signs of keratitis, which presents with severe photophobia, blurred or impaired vision, and a foreign body sensation with difficulty opening the affected eye. Penlight examination reveals a corneal opacity or infiltrate. When keratitis is suspected, the patient should be seen urgently by an ophthalmologist to confirm the diagnosis and begin treatment.
The diagnosis of keratitis is made by slit-lamp examination showing corneal ulceration. The epithelial injury is readily visible with fluorescein. Cultures of corneal scraping should be obtained to help guide definitive antibiotic therapy. While those cultures are processing, empiric therapy should be changed to topical, combination antibiotic therapy that has broad-spectrum activity against gram-positive and gram-negative organisms, including Pseudomonas. Keratitis can cause scarring or ulceration of the cornea and subsequent blindness if not aggressively treated.
Bacterial keratitis (BK) is the most common infectious complication of contact lens use, especially in patients who use extended-wear or overnight lenses. Symptoms include pain, eyelid swelling, photophobia, and conjunctival injection. If the corneal lesion (visible under fluorescein staining) is central, vision may also be affected. An inflammatory infiltrate (hypopyon) is occasionally seen in the anterior chamber.
The diagnosis of BK is primarily clinical. Treatment with empiric, broad-spectrum topical antibiotics (with Pseudomonas coverage) such as the fluoroquionolone gatifloxacin should be initiated; erythromycin would not provide appropriate coverage (Choice D). Culture (via corneal scrapings) or impression cytology is helpful in severe infections or those that fail to respond to initial antibiotic treatment (Choice B). Antibiotics should be applied hourly for the first 24-48 hours, and concomitant corticosteroids should be avoided in the acute phase (Choice C).
Endophthalmitis
Endophthalmitis is a bacterial infection of the deep eye (vitreous) due to either direct inoculation into the globe (eg, surgery, trauma) or hematogenous spread. It is not a complication of bacterial conjunctivitis.